At the first-ever Apache Junction Health and Dental Fair, Stephanie Kok found more than free health screenings — she found inspiration.
By Laura Hahnefeld
Director of Communications, Arizona Alliance for Community Health Centers
Stephanie Kok regards the rock painting she’s just completed: three flowers with lavender petals popping out from bright green stems with tiny round leaves. To fit the shape of the stone, the flowers are painted in varying heights.
She gently places her creation next to several others on a picnic table at the Earth Heart Park & Community Garden, part of Horizon Health and Wellness in Apache Junction, where the first-ever Apache Junction Health and Dental Fair is in full swing. Like many of the attendees from this rural town 35 miles east of Phoenix, Stephanie’s enjoying creative time outdoors after taking advantage of the Jan. 25 fair’s free services inside the health center — services like dental exams, blood pressure and blood sugar checks, fall prevention education, and medication management assistance.
“I love flowers,” says Stephanie, who grew up among the famed tulips of Holland, Michigan. Stephanie reminisces about high school and swimming in Lake Michigan. But growing up wasn’t easy for her.
“I’ve had such a battle with my mental health starting when I was 5 or 6,” she says. “I was in and out of hospitals a lot.”
Now 42, Stephanie says she’s in a much better place. She credits much of her mental and physical health progress to the staff of Horizon Health and Wellness, the community health center she walked into 12 years ago after moving with her parents to Apache Junction and taking a job in a group home.
“Everyone here treats you with the utmost respect,” she says. “Like you’re a human and not just another client.”
A Crucial Link to Care

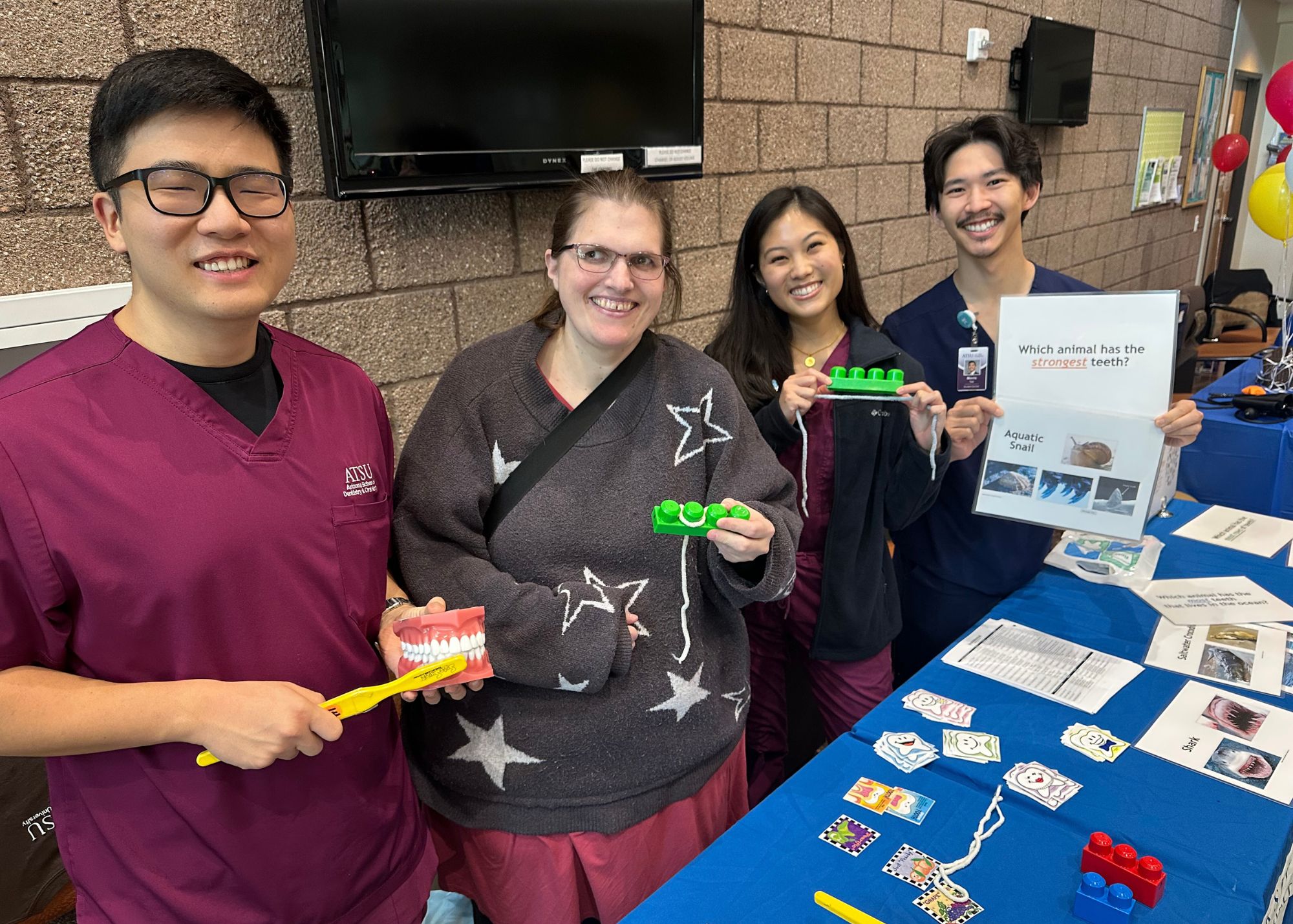
Stephanie Kok receives a dental screening from Kevin Park, a student at A.T. Still University’s Arizona School of Dentistry & Oral Health.
Stephanie says she enjoys the integrated care she receives at Horizon, from primary care to mental health services like counseling and peer support. “I don’t have to travel everywhere, the mental health aspect is here, and my case manager knows me inside and out.”
Horizon Health and Wellness is a nonprofit community health center, a local clinic serving hard-to-reach populations with limited access to health care. Community health centers have become the largest primary health care system in the United States, serving millions of people. In 2023, they provided over 837,000 Arizonans with affordable primary care. Horizon, with nine locations across the state, served nearly 15,000 of them.
In addition to treating the community’s medical, dental, mental health, substance use, and other health care needs, the team at Horizon also addresses another social driver of health in the area: hunger.
“People in Apache Junction are very open, very kind, and there is a growing homeless population,” says Melanie Dunn, Horizon’s talent acquisition specialist. “That’s where our garden comes in. Whatever we harvest goes back to the community. Anyone can take it. But it’s been a hard winter and the quails are punks. They eat everything.”
A Host of Scholars
Inside at the health fair, Stephanie walks from table to table piled high with health and community information – as well as fun freebies like stickers, stress toys, and pill boxes shaped like orange slices. Behind each table are people ready to help. One woman conducts free blood pressure checks. Another helps a client understand her medication regimen. Even a representative from the Apache Junction Public Library is on hand – her book earrings a dead giveaway.
Stephanie’s favorite was the dental table. There, students from A.T. Still University’s Arizona School of Dentistry & Oral Health, in nearby Mesa, demonstrate the correct way to floss using string and oversize Lego-like blocks.
Stephanie Kok (second from left) with students from A.T. Still University’s Arizona School of Dentistry & Oral Health.
“People were so informative,” Stephanie says. “They helped me remember that it’s important to take care of your health – your overall health. Sometimes when you’re struggling with mental health issues, you don’t take care of your physical health.”
Most of the fair’s health representatives double as hosts of the event. They are students participating in the Central Arizona Area Health Education Center (CAAHEC) Scholars Program, one of six sub-recipients of the Area Health Education Center (AHEC) grant in Arizona. CAAHEC is a division of the Arizona Alliance for Community Health Centers (AACHC), the primary care association (PCA) for Arizona. Its two-year interprofessional Scholars Program offers community-based training in underserved areas across Arizona’s AHEC regions.
“The fair wouldn’t have happened without the scholars,” says Mallika Peddada, CAAHEC outreach and development program manager. “Through our program’s immersion process, the students looked at the needs of the Apache Junction community, then worked with the team at Horizon Health to make it happen.”
Mallika says she’s pleased with the fair’s turnout, especially by the number of older adults, some of whom may have never seen a doctor.
“The importance of health fairs is that people can go and get checked by a professional – and that they won’t be judged. It’s good for them and great practice for the students, who are in the health profession.”
Mallika says she’s also impressed by the support the fair received from the Apache Junction community. From garden volunteers passing out seed packets to the town’s fire and police departments stopping by to, you guessed it, rock painting pros.
A New Chapter for Mental Health
As the Apache Junction Health and Dental Fair comes to a close, Stephanie declares it a good day. She had a dental screening. Her blood pressure and blood sugar levels checked out. She learned the correct way to floss. She painted a rock and made it look cool.

Stephanie Kok (left) with Margee Ripley of A.J. Rocks.
And at this point in her mental health journey, she’s ready to give back.
Inspired by the help she received from the peer support program at Horizon Health, Stephanie’s decided to become a peer support for others. The training program is two weeks. She’s submitted her application. She’s excited.
“I want to help others not have to go through what I did,” she says. “The most important thing is to be aware of your diagnosis and educate yourself.”
Sources: Economic Impact of Community Health Centers in the United States, National Association of Community Health Centers (NACHC), March 2023. 2023 Arizona Health Center Program Uniform Data System (UDS) Data